>Sir Alexander Fleming and his discovery of Penicillin
“One sometimes finds what one was not looking for.
Nature makes penicillin; I just found it.”
Sir Alexander Fleming, FRS, FRSE, FRCS (6 August 1881 - 11 March 1955) was a Scottish physician, microbiologist and pharmacologist. His best-known discoveries are the enzyme lysozyme in 1923 and the world's first antibiotic substance, benzylpenicillin (Penicillin_G) from the mould Penicillium notatum in 1928, for which he shared the Nobel Prize in Physiology or Medicine in 1945 with Howard Florey and Ernst Boris Chain. He wrote many articles on bacteriology, immunology, and chemotherapy. His discovery of antibiotics changed medicine and for over 70 years countless lives have been saved. On average antibiotics add 20 years to each person’s life.
More about his life: https://www.nobelprize.org/prizes/medicine/1945/fleming/biographical

FRS, FRSE, FRCS
>Antimicrobial Resistance: The Role of Regulation

April 2019. A Policy Brief: Report on Workshop. Alexandra Ming, Jacob Puddle, Henry Wilson. What role does regulation play in tackling #AMR? The UK Department of Health and Social Care, University College London and Global Governance Institute brought together experts from across disciplines to discuss. https://www.ucl.ac.uk/global-governance/sites/global-governance/files/antimicriobial_resistance_the_role_of_regulation_final_report.pdf
Antimicrobial resistance, or AMR, is one of the most complex and urgent issues facing the world today. Drug-resistant infections already contribute significantly to mortality and morbidity worldwide. If we fail to act soon, by 2050 AMR could lead to more deaths each year than currently caused by cancer. But this is not only a human health issue. Unchecked, #AMR will have devastating consequences on the global economy, food security and agricultural livelihoods, and will undoubtedly jeopardise the achievement of the #SDGs. Medication
A complex, multi-sectoral issue requires a multifaceted response. One component of this response is regulation. Concerted action from around the world has brought us some real triumphs in this area, the peak of which was 193 Member States signing up to the UN political declaration on AMR in 2016. But clearly commitments need to be followed up with tangible action. Regulation can promote policy implementation by enabling the right incentives and disincentives. Take industry, for example. Regulation can be used to push industry to take measures to control the amount of active pharmaceutical ingredient that companies release into waterways. On the other hand, harmonising regulatory pathways for new drugs could incentivise industry to bring new products to market. Foreword: Prof. Dame Sally Davies, CMO
>‘Superbug gene’ found in one of the most remote places on earth
Published on: 28 January 2019. Pub:Environment International. International team of experts from the Universities of Newcastle, York and Kansas and the Chinese Academy of Science in Xiamen. Funded by UK Natural Environmental Research Council and other agencies.

Antibiotic-Resistant Genes (ARGs) that were first detected in urban India have been found 8,000 miles away in one of the last ‘pristine’ places on earth, a new study has shown.
"This finding has huge implications for global AR spread...A clinically important ARG originating from South Asia is clearly not ‘local’ to the Arctic. "Professor David Graham, Newcastle University
Soil samples taken in the Kongsfjorden region of Svalbard have now confirmed the spread of blaNDM-1 into the High Arctic – an ARG originally found in Indian clinical settings, which confer multidrug resistance (MDR) in microorganisms.
Worldwide spread of blaNDM-1 and other ARGs is a growing concern because they often target “last resort” classes of antibiotics, including Carbapenems. Carried in the gut of animals and people, the research team, led by Newcastle University’s Professor David Graham, say the blaNDM-1 and other medically-important ARGs that were found in Arctic soils were likely spread in the faecal matter of migratory birds, other wildlife and human visitors to the area.
Last pristine ecosystems on earth
“Polar regions are among the last presumed pristine ecosystems on Earth, providing a platform for characterizing pre-antibiotic era background resistance against which we could understand rates of progression of AR ‘pollution’,” says Professor Graham, an environmental engineer at Newcastle University who has spent 15 years studying the environmental transmission of antibiotic resistance around the world. “But less than three years after the first detection of the blaNDM-1 gene in the surface waters of urban India we are finding them thousands of miles away in an area where there has been minimal human impact. Encroachment into areas like the Arctic reinforces how rapid and far-reaching the spread of antibiotic resistance has become, confirming solutions to AR must be viewed in global rather than just local terms.”
>New International Reference Centre for AMR launched by the Fleming Fund
https://www.flemingfund.org/publications/the-fleming-fund-launches-the-international-reference-centre-for-antimicrobial-resistance-amr/
20 November 2018. Dame Sally Davies announced that the Fleming Fund is providing £1m to support this new international reference centre which will provide technical assistance and quality assurance in one-health surveillance.
>New International Centre for Interdisciplinary Solutions on AMR
https://ufm.dk/en/newsroom/news/2018/denmark-to-host-new-international-research-center-for-global-solutions-on-antimicrobial-resistance
15 November 2018. The Danish government announced an important step in the the process of strengthening global governance in the fight against AMR when it signed a MOU with Consultative Group on International Agricultural Research (CGIAR). The agreement states mutual intentions to collaborate closely on the establishing an independent research centre, the International Centre for Interdisciplinary Solutions on AMR, in Denmark.
The Copenhagen centre will act as an independent global knowledge node for generating, aggregating and disseminating evidence on antimicrobial drug resistance. It has a starting budget of $10m, 75% of which is coming from the Danish government. This will go up to $35m in 2023 and will be largely financed by international donors.
>OECD: Stemming the Superbug Tide - Just A Few Dollars More
Published 07 November 2018. OECD Health Policy Studies.
Buy or read online: http://www.oecd.org/health/stemming-the-superbug-tide-9789264307599-en.htm

Antimicrobial resistance (AMR) is a large and growing problem with the potential for enormous health and economic consequences, globally. As such, AMR has become a central issue at the top of the public health agenda of OECD countries and beyond. In this report, OECD used advanced techniques, including machine learning, ensemble modelling and a microsimulation model, to provide support for policy action in the human health sector. AMR rates are high and are projected to grow further, particularly for second- and third-line antibiotics, and if no effective action is taken this is forecasted to produce a significant health and economic burden in OECD and EU countries.
This burden can be addressed by implementing effective public health initiatives. This report reviews policies currently in place in high-income countries and identifies a set of ‘best buys’ to tackle AMR that, if scaled up at the national level, would provide an affordable and cost-effective instrument in the fight against AMR.
 >PODCAST: Tackling the AMR Crisis
>PODCAST: Tackling the AMR Crisis
Listen to the podcast: https://scrip.pharmaintelligence.informa.com/SC123501/Podcast-Tackling-The-AMR-Crisis
The issue of antimicrobial resistance (AMR) has been stalking global public health for a number of years – and governments, health authorities and the international scientific community as a whole is finally starting to take action. In this podcast Mike Ward of Informa talks to Dr Peter Jackson, executive director of the AMR Centre, a public-private partnership, which is based at Alderley Park, Cheshire, and leads the UK response to the crisis.
>Access to Medicine Foundation
https://amrbenchmark.org/ Download the White Paper: https://amrbenchmark.org/wp-content/uploads/2018/04/Antimicrobial-Resistance-Benchmark-2018.pdf
31 May 2018. New white paper unpacks systemic causes of antibiotic shortages and calls for global action to rebuild the market Access to Medicine Foundation warns that antibiotic supply chains are on the brink of collapse, putting basic healthcare at risk, in a new white paper titled “Shortages, stockouts and scarcity: the issues facing the security of antibiotic supply and the role for pharmaceutical companies”. Urgent action is needed to rebuild the antibiotics market. The paper shows how some pharmaceutical companies are responding.
>The Antimicrobial Resistance Benchmark from Access to Medicine Foundation
https://amrbenchmark.org/ Download the AMR Benchmark https://amrbenchmark.org/wp-content/uploads/2018/04/Antimicrobial-Resistance-Benchmark-2018.pdf
January 2018. Key Findings: https://amrbenchmark.org/wp-content/uploads/2017/12/AMRB2018-Key-Findings.pdf. The Antimicrobial Resistance Benchmark provides the first assessment of how pharmaceutical companies are tackling the threat of antimicrobial resistance (AMR). The 30 companies in scope include those with the largest R&D divisions, the largest market presence, and specific expertise in developing critically needed medicines and vaccines.
The goal of the Antimicrobial Resistance Benchmark is to guide and incentivise pharmaceutical companies to adopt and implement effective actions for tackling the problem of AMR. It highlights where good ideas for limiting AMR are being implemented and where action is still required.
>The Longitude Prize
In order to tackle growing levels of antimicrobial resistance, the challenge set for the Longitude Prize is to invent an affordable, accurate, fast and easy-to-use test for bacterial infections that will allow health professionals worldwide to administer the right antibiotics at the right time.
https://longitudeprize.org/challenge
>Everyone Needs to be an Antibiotic Resistance Fighter
19 January 2018 Written by Daniel Evans, University of Pittsburgh
https://longitudeprize.org/blog-post/everyone-needs-be-antibiotic-resistance-fighter

Longitude Prize: Infectious Futures
In 2015, six stories were commissioned about a future facing up to the challenge of antibiotic resistance called Infectious Futures: Stories of the post-antibiotic apocalypse as part of a much larger effort to publicise, educate, and enrich the conversation around the subject. These stories, originally in print form, will be uploaded as blogs, one at a time into an online collection. Enjoy!
https://longitudeprize.org/antimicrobial-resistance/infectious-futures-stories-post-antibiotic-apocalypse
>The FAO action plan on Antimicrobial Resistance 2016-2020
www.fao.org/3/a-i5996e.pdf
Supporting the food and agriculture sectors in implementing the Global Action Plan on Antimicrobial Resistance to minimize the impact of antimicrobial resistance (available in French and Spanish)
>21 September 2016 - Draft 'POLITICAL DECLARATION' of the high-level meeting of the UN General Assembly on antimicrobial resistance
>WHO Director-General addresses UN General Assembly on Antimicrobial Resistance - and says consumers should choose antibiotic-free meat
http://www.who.int/dg/speeches/2016/unga-antimicrobial-resistance/en/
21 September 2016. New York, USA
Dr Margaret Chan, Director-General of the World Health Organization
“The food industry needs to reduce its massive use of antibiotics, at sub-therapeutic doses, as growth promoters. Specific antibiotics, listed by WHO as critically important for human medicine, should not be used in animal husbandry or agriculture.”
“Consumers should make antibiotic-free meat their preferred choice.”
>G20 Leaders’ Communique Hangzhou Summit
Hangzhou, 5 September 2016 . http://europa.eu/rapid/press-release_STATEMENT-16-2967_en.htm
Antimicrobial resistance (AMR) poses a serious threat to public health, growth and global economic stability. The Communique affirms the need to explore in an inclusive manner to fight antimicrobial resistance by developing evidence-based ways to prevent and mitigate resistance, and unlock research and development into new and existing antimicrobials from a G20 value-added perspective, and call on the WHO, FAO, OIE and OECD to collectively report back in 2017 on options to address this including the economic aspects.
White Blood Cells
 >Minister questioned on Government's Antimicrobial Resistance Strategy
>Minister questioned on Government's Antimicrobial Resistance Strategy
WATCH UK Parliament TV 11 September 2018. Antimicrobial resistance
The Health and Social Care Committee hears from Steve Brine MP, Parliamentary Under Secretary of State, Department of Health and Social Care, and healthcare professionals, on priorities for the Government’s next AMR strategy.
 >Antimicrobial Resistance Inquiry
>Antimicrobial Resistance Inquiry
WATCH UK Parliament TV 4 September 2018 Health and Social Care Committee
Witnesses: Professor Dame Sally Davies, Chief Medical Officer for England, Lord O'Neill of Gatley, Christine Middlemiss, Chief Veterinary Officer, Government Veterinary Services.
>NHS is hiding the true scale of deaths caused by drug-resistant infections out of fear the health service will look bad
04.09.18 Speaking to the UK Government's Health Select Committee, Dame Sally said that without antibiotics, modern medicine will be 'lost'. She called for a rule change to make sure it is routinely recorded on people's death certificates if they died of an antibiotic-resistant infection. She said: 'That would really wake people up to the deaths as they happen,' 'One of the problems at the moment is families often don’t know that their bereavement was due to infection,' Dame Sally added. 'And they’re rarely told that the infection was resistant to treatment because it looks as if the NHS is failing.' Read more The Telegraph.

>ESPAUR REPORTS
English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR). The reports include data on antimicrobial consumption in primary and secondary care. This data should be used by commissioners and health organisations to benchmark against national and regional antibiotic resistance and prescribing, and determine appropriate local action. This monitors the way antibiotics are prescribed and obtained from pharmacies across the NHS in England.
>ESPAUR: Report 2018
https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report
23.October 2018. Updated. Ref: PHE publication gateway reference: 2018533PDF, 2.2MB, 147 pages
The 2018 Report highlights how more than 3 million common procedures such as cesarean sections and hip replacements could become life-threatening without them. Without antibiotics, infections related to surgery could double, putting people at risk of dangerous complications. Cancer patients are also much more vulnerable if antibiotics don’t work; both cancer and the treatment (chemotherapy) reduce the ability of the immune system to fight infections. Antibiotics are critical to both prevent and treat infections in these patients
The threat of antibiotic resistance continues to grow. Bloodstream infections have increased and the report shows that antibiotic-resistant bloodstream infections rose by an estimated 35% between 2013 and 2017.
Despite the risks of antibiotic resistance, research shows that 38% of people still expect an antibiotic from a doctor’s surgery, NHS walk-in centre or ‘GP out-of-hours’ service when they visited with a cough, flu or a throat, ear, sinus or chest infection in 2017.
>ESPAUR Report 2017: executive summary
The ESPAUR report includes national data on antibiotic prescribing and resistance, and hospital antimicrobial stewardship implementation.
The ESPAUR report:
- shows developments in antimicrobial stewardship and professional or public education and awareness activities
- reviews ESPAUR activities
- highlights progress made in the previous year
The 2017 report details trends on antimicrobial usage and resistance, covering the years 2012 to 2016.
It sets a standard to compare antimicrobial use and resistance in successive years and acts as a resource for commissioning and implementing antimicrobial stewardship policies in England. The ESPAUR report addresses important aspects of the UK 5-year antimicrobial resistance (AMR) strategy.
>Northern Ireland tops UK for antibiotic prescribing | Antimicrobial stewardship
27.10.17. https://www.pharmaceutical-journal.com/news-and-analysis/news-in-brief/northern-ireland-tops-uk-for-antibiotic-prescribing/20203812.article
Northern Ireland’s antibiotic use is the highest in the UK with prescribing rates currently 30% higher than in England, according to Michael McBride, chief medical officer for the country. Most antibiotics prescriptions were issued by GPs, but 8% were prescribed by dentists.
In his latest annual report, Your Health Matters, McBride said that while there has been a 10% reduction in antibiotic prescribing over the last ten years, Northern Ireland still needs to take urgent steps to preserve the drugs’ efficacy.
To that end, he said that during 2016–2017 more than half of Northern Irish GP practices allocated a member of staff to become an ‘antibiotic champion’, and that during 2017–2018 several GP practices will pilot finger-tip blood tests to distinguish between bacterial and viral infections. He added that prescription levels in dental practice were also being looked at.
McBride highlighted the part that Northern Ireland’s pharmacists play in antimicrobial stewardship, pointing out that “modern pharmacists’ roles involve prescribing, medication reviews, advising medical and nursing staff and patients on the safe and appropriate use of medicines, as well as supplying medicines”.
He also said that he had previously worked with Mark Timoney, Northern Ireland’s chief pharmaceutical officer, to produce the Northern Ireland Medicines Optimisation Quality Framework, which makes recommendations to promote better use of medicines, including antibiotics.
Citation: The Pharmaceutical Journal, PJ October 2017 online, | DOI: 10.1211/PJ.2017.20203812
>Antimicrobial stewardship
21 August 2017. https://www.nursingtimes.net/clinical-archive/infection-control/reducing...
A national guideline on antimicrobial stewardship has been published by the National Institute for Health and Care Excellence (NICE). This recommends developing systems to provide regular updates to individual prescribers and prescribing leads on individual prescribing. These are benchmarked against local and national antimicrobial prescribing rates and trends collated by PHE.
> Infection prevention and control commissioning toolkit
Infection prevention and control commissioning toolkit
January 2016 2nd edition PDF.
The document was produced by the RCN and the Infection Prevention Society (IPS) and will be reviewed again in 2019.
https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
The toolkit supports the commissioning of infection prevention and control as a resource for both commissioner and provider organisations. It includes a basket of indicators that can be used or adapted at local level to meet local needs and support ongoing improvement in HCAI reduction. The indicators have been mapped against the UK 5 year antimicrobial resistance strategy and are reported on annually.
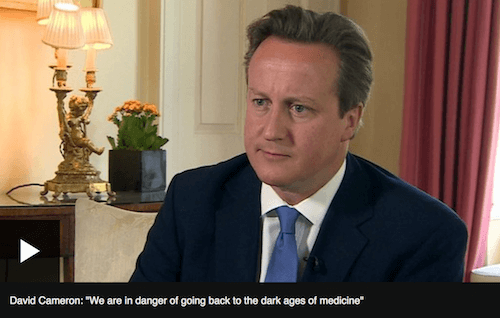
>Antibiotic resistance: Prime Minister Cameron commissions a review on AMR
and warns of medical 'dark ages' 2 July 2014 https://www.bbc.co.uk/news/health-28098838
"If we fail to act, we are looking at an almost
unthinkable scenario where antibiotics
no longer work and we are cast back
into the dark ages of medicine"
David Cameron, UK Prime Minister. (2014)
The wide-ranging REVIEW was commissioned in July 2014 by the then UK Prime Minister, David Cameron, who asked economist Jim O’Neill to analyse the global problem of rising drug resistance and propose concrete actions to tackle it internationally. The Review on AMR was jointly supported by the UK Government and Wellcome Trust, although operated with full independence from both. Established as a two-year, time-limited process, the Review engaged widely with international stakeholders to understand and propose solutions to the problem of drug-resistant infections from an economic and social perspective, and produced its final report and recommendations in the summer of 2016.
The Review on Antimicrobial Resistance has now completed its work. The content of this website is frozen as an archive of the Review’s work, and will not be updated further. The legacy of the Review will be maintained by its sponsor organisations, the Wellcome Trust and the UK Department of Health. To view video: https://www.bbc.co.uk/news/health-28098838
>UK 5 Year Antimicrobial Resistance (AMR) Strategy - Measuring Success
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/322358/Outcome_measures.pdf 10 pages
23 June 2014. The measures agreed by the UK antimicrobial resistance strategy High Level Steering Group, taking advice from expert scientific advisory committees including the Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infections (ARHAI), cover 4 areas:
- trends in resistance
- quality of prescribing in primary and secondary healthcare settings
- public and professional knowledge and understanding of antimicrobials and their appropriate use.
- global security through ensuring global alignment in addressing AMR
These measures apply equally to human and animal health.
>UK Five Year Antimicrobial Resistance Strategy 2013 to 2018
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/244058/20130902_UK_5_year_AMR_strategy.pdf
September 2013. There are few public health issues of greater importance than antimicrobial resistance (AMR) in terms of impact on society. This problem is not restricted to the UK. It concerns the entire world and requires action at local, national and global level. AMR cannot be eradicated but a multidisciplinary approach involving a wide range of partners will limit the risk of AMR and minimise its impact for health, now and in the future.
The harsh reality is that infections are increasingly developing that cannot be treated. The rapid spread of multi-drug resistant (MDR) bacteria means that we could be close to reaching a point where we may not be able to prevent or treat everyday infections or diseases. Many existing antimicrobials are becoming less effective. Bacteria, viruses and fungi are adapting naturally and becoming increasingly resistant to medicines used to treat the infections they cause. Inappropriate use of these valuable medicines has added to the problem. Coupled to this, the development pipeline for new antibiotics is at an all-time low. We must therefore conserve the antibiotics we have left by using them optimally. The process of developing new antimicrobials and new technologies to allow quicker diagnosis and facilitate targeted treatment must be accelerated. Information resources also need to be strengthened to support health professionals, their patients, animal keepers and the public, so that all understand the value and importance of antibiotics to society.
>Antibiotics - the disappearing miracle drugs
V3PressRelease18.11.13.pdf
Published by CombatAMR.org on 6th August 2014 to mark Alexander Fleming’s Birthdate