>Antibiotic Discovery: Where Have We Come from, Where Do We Go?
24 April 2019. Bernardo Ribeiro da Cunha,Luís P. Fonseca and Cecília R. C. Calado
Antibiotics 2019, 8(2), 45; https://doi.org/10.3390/antibiotics8020045
Abstract Given the increase in antibiotic-resistant bacteria, alongside the alarmingly low rate of newly approved antibiotics for clinical usage, we are on the verge of not having effective treatments for many common infectious diseases. Historically, antibiotic discovery has been crucial in outpacing resistance and success is closely related to systematic procedures—platforms—that have catalyzed the antibiotic golden age, namely the Waksman platform, followed by the platforms of semi-synthesis and fully synthetic antibiotics. Said platforms resulted in the major antibiotic classes: aminoglycosides, amphenicols, ansamycins, beta-lactams, lipopeptides, diaminopyrimidines, fosfomycins, imidazoles, macrolides, oxazolidinones, streptogramins, polymyxins, sulphonamides, glycopeptides, quinolones and tetracyclines. During the genomics era came the target-based platform, mostly considered a failure due to limitations in translating drugs to the clinic. Therefore, cell-based platforms were re-instituted, and are still of the utmost importance in the fight against infectious diseases. Although the antibiotic pipeline is still lackluster, especially of new classes and novel mechanisms of action, in the post-genomic era, there is an increasingly large set of information available on microbial metabolism. The translation of such knowledge into novel platforms will hopefully result in the discovery of new and better therapeutics, which can sway the war on infectious diseases back in our favor. Full article
>ECDC: Continuing its Strategic Multi-annual Programme & will produce a new long-term strategy
11th January 2019. Single programming document 2019–2021

In the wake of the 2017 Rome Declaration for a strong and secure Europe in the world, and based on the provisions of Article 168 of the European Treaty, ECDC’s role and contribution has become even more essential because of the shared responsibility between the EU and the Member States to protect and improve human health against major cross-border threats. In 2019, ECDC will continue to contribute to health security, including particular attention to
- Tackle antimicrobial resistance
- Improve vaccine coverage in the EU
In 2019 and 2020, ECDC will continue to implement its Strategic Multi-annual Programme 2014–2020 (SMAP). The SMAP – after a 2016 mid-term review by the Management Board – was integrated in the multiannual section of the Single Programming Document. ECDC will also produce a new long-term strategy that will guide the Centre’s efforts for the years ahead; implementation is scheduled for 2021. This strategy will draw on the results of ECDC third external evaluation covering the years 2012–2017, launched in 2018 and completion expected in 2019. Other input will incorporate other evaluations from the ECDC surveillance systems (EPHESUS project), ECDC’s Disease Programmes, and the ECDC Fellowship Programme. In this context, the Single Programming Document constitutes an essential element for the guidance of ECDC’s work and its resource allocation.
>WHO Guidelines on Hand Hygiene in Healthcare
The WHO guidelines on hand hygiene in health care provide health-care workers (HCWs), hospital administrators and health authorities with a thorough review of evidence on hand hygiene in health care and specific recommendations to improve practices and reduce transmission of pathogenic microorganisms to patients and HCWs.
The present guidelines are intended to be implemented in any situation in which healthcare is delivered either to a patient or to a specific group in a population. Therefore, this concept applies to all settings where healthcare is permanently or occasionally performed. English. 270 pages. ISBN: ISBN 978 92 4 159790 6 WHO reference number: WHO/IER/PSP/2009/01. WHO Guidelines on Hand Hygiene in Health Care. Summary of WHO guidelines on hand hygiene in health care (English)
>World Health Organization (WHO) What are the core components for effective infection prevention and control?
This instructional video from the World Health Organization explains the evidence-based core components of infection prevention and control programmes, critical at both the national and acute health care facility level for patient safety and for health systems to provide quality care. This video is brought to life by interviews from people in the field across a range of countries and describes the importance of the eight core components one by one. It will be a great addition to health care training sessions and the information is a key part of the infection prevention and control implementation and improvement process.
For more information and tools: www.who.int/infection-prevention/tools/core-components/en/

>New edition of the WHO global guidelines for the prevention of surgical site infections
https://www.who.int/infection-prevention/publications/ssi-prevention-guidelines/en/.The December 2018 edition of the guidelines includes the revision of the recommendation regarding the use of 80% fraction of inspired oxygen (high FiO2) in surgical patients under general anaesthesia with tracheal intubation and the update of the section on implementation.
In addition, a new Implementation manual to support the prevention of surgical site infection at the facility level: turning recommendations into practice is available.
>A look back at a year of vaccine announcements
12 January 2019. Since Access to Medicine Foundation published the Access to Vaccines Index in March 2017, vaccine companies have reported a series of positive developments in their efforts to address immunisation coverage. The Access to Medicine Foundation has reviewed these statements to give a sense of the level of momentum in the vaccines industry to improve access to vaccines. Download the Overview of the companies public announcements.
The overview published today summarises announcements made by the eight companies evaluated in the Access to Vaccines Index. It includes announcements published between 1 April 2017 and 3 January 2018. Out of 18 published announcements, two thirds relate to research and development, with others relating to licensing agreements, procurement matters and vaccine supply.
Vaccine companies report more activity in research and development than in other areas, making nine announcements relating to clinical trials and four about new R&D partnerships that aim to make vaccines more effective or easier to deploy to limited-resource communities. An announcement regarding a technology transfer supports the view that licensing is a feasible and effective way of increasing access to vaccines. More companies can take advantage of licensing as a way of introducing their vaccines in new markets. Three companies announced developments that can help make vaccine supply more reliable, including for pneumonia, influenza and polio vaccines.
>6th Access to Medicine Index
20 November 2018. It evaluates 20 of the world's largest pharmaceutical companies on their actions to improve access to medicine. The Index covers 106 low- and middle-income countries and 77 diseases, conditions and pathogens. The 2018 Index provides a finely detailed picture of these companies’ access-related policies and practices based on an analysis of 69 indicators, concerning 106 low- and middle-income countries and 77 diseases, conditions and pathogens.
>UN Environment Programme joins the Tripartite Plus
http://www.fao.org/news/story/en/item/1169662/icode/
12 November 2018 Bangkok, Thailand
The global tripartite partnership calling for more responsible use of antibiotics in humans, animals and agriculture (including aquaculture and plant production) has announced it is widening its coverage to include the environment sector.
The Food and Agriculture Organization of the United Nations (FAO), World Organisation for Animal Health (OIE), and World Health Organization (WHO) have expanded their partnership to counter antimicrobial resistance (AMR) through the addition of the United Nations Environment Programme (UN Environment). The move is intended to attack AMR in a more holistic way. The new partnership, which will be known as the Tripartite Plus, was announced today at the opening of the World Antibiotic Awareness Week (WAAW) observance in Asia and the Pacific.
>2018 Tripartite Report
http://www.fao.org/3/ca0486en/CA0486EN.pdf
MONITORING GLOBAL PROGRESS ON ADDRESSING ANTIMICROBIAL RESISTANCE
Analysis report of the second round of results of AMR country self-assessment survey 2018,
Published by the Food and Agriculture Organization of the United Nations, the World Organisation for Animal Health and the World Health Organization. The report reflects progress in the human, animal (terrestrial and aquatic), plant, food safety and environmental sectors. 154 countries out of 194 WHO Member States responded to this round of the self-assessment survey – a response rate of 79.4%. It outlines the progress achieved towards the goals of the Global Action Plan.
>Global Action Plan on Antimicrobial Resistance -
Message from WHO Director-General, Dr Tedros Adhanom Ghebreyesus

18.07.18 http://www.who.int/news-room/detail/18-07-2018-countries-step-up-to-tack...
Countries are making significant steps in tackling antimicrobial resistance (AMR), but serious gaps remain and require urgent action, according to a report released today by the Food and Agriculture Organization of the United Nations (FAO), World Organisation for Animal Health (OIE) and the World Health Organization (WHO). The report charts progress in 154 countries and reveals wide discrepancies.
>Antimicrobial resistance and our food systems: challenges and solutions
http://www.fao.org/3/a-i6106e.pdf
Global food production has intensified over the past 50 years due to economic expansion and population growth. The use of antimicrobials in agriculture – in livestock, fish farming, and even on crops – has grown as well. Antimicrobials are not only used as medicines, but are sometimes also added in low concentrations to animal feed as a way of stimulating growth.
>Why we need a World Food Safety Day
http://www.fao.org/fao-who-codexalimentarius/news-and-events/news-detail...
Sufficient amounts of safe and nutritious food is essential to human health but it is also important to acknowledge the strong links between food and health, since the World Health Organisation estimates that foodborne hazards are responsible for 600 million cases of foodborne diseases and 420,000 deaths globally every year. Having an international day would highlight the burden unsafe food places on health, communities and economies. It would provide an opportunity to underscore the fundamental role food safety has in achieving the Sustainable Development Goals (SDGs) and strengthen international efforts to ensure that the food we eat is safe.
“I encourage all Codex Members and Observers and anyone else who would like to participate in this campaign to bring world attention to the importance of food safety! We need food to live – safe food, and we have to care about keeping it safe”
Tom Heilandt, Codex Secretary
>Third Progress report on the UK 5 year AMR strategy: 2016 - GOV.UK
www.gov.uk/government/publications/progress-report-on-the-uk-5-year-amr-...
24.11.2017 https://www.gov.uk › Health and social care › Health improvement
The third annual progress report on the UK 5 year antimicrobial resistance (AMR)strategy, including future plans.
>New work underway by Codex Alimentarius on surveillance and code of practice for foodborne antimicrobial resistance
28.07.2017 http://www.fao.org/antimicrobial-resistance/news-and-events/news/news-de...

New work on antimicrobial resistance (AMR) was approved by the Codex Alimentarius Commission (CAC) at its 40th Session in Geneva 17 to 22 July 2017. The Commission agreed to developing Guidance on Integrated Surveillance of Antimicrobial Resistance, and revising its 2005 Code of Practice to Minimise and Contain Antimicrobial Resistance.
The Codex Alimentarius works to protect consumer health and ensure fair food trade practices and is a joint initiative of the Food and Agriculture Organization of the United Nations (FAO), and the World Health Organization (WHO).
FAO, together with its tripartite colleagues in WHO and OIE, updated member countries on their ongoing and future work on AMR during the Commission and at a special AMR side event on 17th July.
Dr Sarah Cahill, a member of FAO’s AMR Working Group and panellist at the AMR side event explained that FAO is working on strengthening governance by providing technical feedback on animal and plant health legislation and guidelines to support capacity development for AMR management at the country level. She also informed delegates that legal information on AMR is being included in FAOLEX (one of the world’s largest and most comprehensive legislative and policy databases on food, agriculture and natural resources management). She also stressed the importance of sharing good practices in food control and agriculture production systems.
Speakers highlighted the need for new data in addition to the existing information on foodborne AMR to support the new Codex work. A call for data will be issued next month and countries are urged to make every effort to respond to this request for new data on AMR to inform the Guidance and Code of Practice.
Professor Yong Ho Park from the Republic of Korea and chairperson of the ad hoc Codex Task Force on Antimicrobial Resistance also invited members to join the task force in its deliberations at Jeju Island in the Republic of Korea on 27 November to 1 December 2017. This meeting will afford an opportunity for countries to directly participate in the development of global guidance and standards related to AMR, ensuring that this work takes into consideration their needs and challenges.
There is widespread agreement on the cause of antimicrobial resistance. Scientists and public authorities acknowledge that overuse and abuse of antibiotics and other antimicrobial drugs – in agriculture and in modern medicine – are the culprit.
>The FAO Action Plan on Antimicrobial Resistance 2016-2020
www.fao.org/3/a-i5996e.pdf
Supporting the food and agriculture sectors in implementing the Global Action Plan on Antimicrobial Resistance to minimize the impact of antimicrobial resistance.
>Water availability at hospitals in low- and middle-income countries: implications for improving access to safe surgical care
Pub. Journal of Surgical Research September 2016 (205) p. 169 e178. Sagar S. Chawla, BS,a, * Shailvi Gupta, MD, MPH,b Frankline M. Onchiri, PhD,c Elizabeth B. Habermann, PhD, MPH,d Adam L. Kushner, MD, MPH,e,f,g and Barclay T. Stewart, MDh,i,j,k
Although two billion people now have access to clean water, many hospitals in low- and middle-income countries (LMICs) do not. Lack of water availability at hospitals hinders safe surgical care. We aimed to review the surgical capacity literature and document the availability of water at health facilities and develop a predictive model of water availability at health facilities globally to inform targeted capacity improvements. Results: Of the 72 records identified, 19 reported water availability representing 430 hospitals. A total of 66% of hospitals assessed had water availability (283 of 430 hospitals). Using these data, estimated percent of water availability in LMICs more broadly ranged from under 20% (Liberia) to over 90% (Bangladesh, Ghana). Conclusions: Less than two-thirds of hospitals providing surgical care in 19 LMICs had a reliable water source. Governments and nongovernmental organizations should increase efforts to improve water infrastructure at hospitals, which might aid in the provision of safe essential surgical care. Future research is needed to measure the effect of water availability on surgical care and patient outcomes.

>CDC Publishes 2016 Healthcare-Associated Infection (HAI) Progress Report
www.cdc.gov/hai/data/portal/progress-report.html
2016. The Centers for Disease Control and Prevention (CDC) has published the 2016 Healthcare-Associated Infection Progress Report (HAI Progress Report). This report shows year-to-year progress on the prevention of key healthcare-associated infections (HAIs) to help highlight progress as well as target areas that need improvement. The 2016 HAI Progress Report is the first report to measure year-to-year HAI prevention progress using the 2015 baseline, or reference point. The baseline was recently updated to take into account advancements in HAI prevention and updated National Healthcare Safety Network (NHSN) definitions. This more current baseline allows for a more realistic and meaningful view of progress.
>Healthcare Associated Infections (HAI): point prevalence survey, England
www.gov.uk/government/publications/healthcare-associated-infections-hcai...
A point prevalence survey on levels of healthcare-associated infections (HAI) and levels of antimicrobial use in hospitals in England in 2016.
> Point Prevalence Surveys
The first national point prevalence survey was completed in the autumn of 2011 and repeated in 2016. The report provides a snapshot of the prevalence of HCAI and levels of antimicrobial usage in hospitals in England at the time of the survey.
The objectives of the point prevalence survey of HAIs and AMU in acute-care hospitals are to:
- estimate the total burden (prevalence) of HAIs and AMU in acute-care hospitals;
- describe patients, invasive procedures, infections (sites, microorganisms including markers of antimicrobial resistance) and antimicrobials prescribed (compounds, indications)
- describe key structures and processes for the prevention of HAIs and antimicrobial resistance at the hospital and ward level in EU hospitals
- disseminate results to those who need to know at local, regional and national levels
>Antimicrobial stewardship
https://www.nursingtimes.net/clinical-archive/infection-control/reducing...
A national guideline on antimicrobial stewardship has been published by the National Institute for Health and Care Excellence (NICE). This recommends developing systems to provide regular updates to individual prescribers and prescribing leads on individual prescribing. These are benchmarked against local and national antimicrobial prescribing rates and trends collated by PHE.
>Infection prevention
Infection prevention and control commissioning toolkit (PDF, 1.44MB, 24 pages) supports the commissioning of infection prevention and control as a resource for both commissioner and provider organisations. It includes a basket of indicators that can be used or adapted at local level to meet local needs and support on-going improvement in HCAI reduction. The indicators have been mapped against the UK 5 year antimicrobial resistance strategy (PDF, 400KB, 43 pages) and are reported on annually.
>European Antimicrobial Resistance Surveillance Network (EARS-Net)
Collects data on invasive bacterial isolates from 30 EU or EEA countries and has published a summary of the latest data on antibiotic resistance in the EU (PDF, 79KB, 8 pages).
>ESPAUR reports (updated 03.11.17)
Reports include data on antimicrobial consumption in primary and secondary care. This data should be used by commissioners and health organisations to benchmark against national and regional antibiotic resistance and prescribing, and determine appropriate local action.
>ESPAUR: Report 2018
https://www.gov.uk/government/publications/english-surveillance-programm...
23.October 2018. Updated. Ref: PHE publication gateway reference: 2018533PDF, 2.2MB, 147 pages
The 2018 Report highlights how more than 3 million common procedures such as cesarean sections and hip replacements could become life-threatening without them. Without antibiotics, infections related to surgery could double, putting people at risk of dangerous complications. Cancer patients are also much more vulnerable if antibiotics don’t work; both cancer and the treatment (chemotherapy) reduce the ability of the immune system to fight infections. Antibiotics are critical to both prevent and treat infections in these patients
The threat of antibiotic resistance continues to grow. Bloodstream infections have increased and the report shows that antibiotic-resistant bloodstream infections rose by an estimated 35% between 2013 and 2017.
Despite the risks of antibiotic resistance, research shows that 38% of people still expect an antibiotic from a doctor’s surgery, NHS walk-in centre or ‘GP out-of-hours’ service when they visited with a cough, flu or a throat, ear, sinus or chest infection in 2017.
>ESPAUR report 2017: executive summary
Ref: PHE publications gateway number 2017491 PDF, 76KB, 5 pages
The ESPAUR report:
- shows developments in antimicrobial stewardship and professional or public education and awareness activities
- reviews ESPAUR activities
- highlights progress made in the previous year
The 2017 report details trends on antimicrobial usage and resistance, covering the years 2012 to 2016.
It sets a standard to compare antimicrobial use and resistance in successive years and acts as a resource for commissioning and implementing antimicrobial stewardship policies in England. The ESPAUR report addresses important aspects of the UK 5-year antimicrobial resistance (AMR) strategy.
>ESPAUR: Full report 2017
Ref: PHE publications gateway number 2017491PDF, 2.92MB, 189 pages
>ESPAUR Report 2016 - Public Health England News and Media
https://phe-newsroom.prgloo.com/resources/espaur-report-2016
17 Nov 2016. Download "ESPAUR Report 2016.pdf" (2.54 MB)
>Review of Evidence on Antimicrobial Resistance and Animal Agriculture in Developing Countries
http://a4nh.cgiar.org/files/2015/06/EoD_Consultancy_June15_Ag_Related_AM... Delia Grace 2015
This report has been produced by the International Livestock Research Institute (ILRI) for Evidence on Demand with the assistance of the UK Department for International Development (DFID) contracted through the Climate, Environment, Infrastructure and Livelihoods Professional Evidence and Applied Knowledge Services (CEIL PEAKS) programme, jointly managed by DAI (which incorporates HTSPE Limited) and IMC Worldwide Limited.
>Fight Antimicrobial Resistance or Go Back to the Pre-Antimicrobial Era
March 2, 2015. (Powerpoint) Mohan P. Joshi, MBBS, MSc, MD Principal Technical Advisor and Cluster Lead for Pharmaceutical Services, MSH/SIAPS Malaika Ludman, MPH Technical Advisor, MSH/SIAPS
Global Health Mini-University March 2, 2015 Washington, DC. Articulates with evidence and examples, the global threat of antimicrobial resistance (AMR) and its consequences, outlining the World Health Organization’s Global Action Plan to Combat AMR and the US government’s National Strategy for the Containment of Antibiotic Resistant Bacteria.
>UK 5 Year Antimicrobial Resistance (AMR) Strategy - Measuring Success
PDF, 214KB, 10 pages Published 23 June 2014
The measures agreed by the UK antimicrobial resistance strategy High Level Steering Group, taking advice from expert scientific advisory committees including the Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infections (ARHAI), cover 4 areas:
- trends in resistance
- quality of prescribing in primary and secondary healthcare settings
- public and professional knowledge and understanding of antimicrobials and their appropriate use.
- global security through ensuring global alignment in addressing AMR.
These measures apply equally to human and animal health.
>The Review on Antimicrobial Resistance (AMR)
https://amr-review.org/
Commissioned in July 2014 by the UK Prime Minister, who asked economist Jim O’Neill to analyse the global problem of rising drug resistance and propose concrete actions to tackle it internationally. The Review on AMR was jointly supported by the UK Government and Wellcome Trust, although operated with full independence from both. Established as a two-year, time-limited process, the Review engaged widely with international stakeholders to understand and propose solutions to the problem of drug-resistant infections from an economic and social perspective, and produced its final report and recommendations in the summer of 2016.
The Review on Antimicrobial Resistance has now completed its work. The content of this website is frozen as an archive of the Review’s work, and will not be updated further. The legacy of the Review will be maintained by its sponsor organisations, the Wellcome Trust and the UK Department of Health. To view video: https://www.bbc.co.uk/news/health-28098838
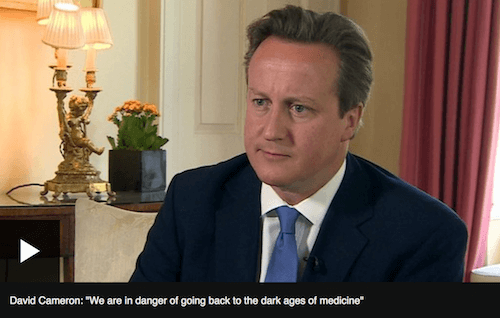
"If we fail to act, we are looking at an almost unthinkable scenario where antibiotics
no longer work and we are cast back into the dark ages of medicine"
David Cameron, UK Prime Minister. (2014)
>Drug War: The Growing Threat for Antimicrobial Resistance
https://rusi.org/system/files/AMR_paper_formatted.pdf
2014. Group Captain Andy Green & Jennifer Cole.
RUSI National Security & Resilience Department.
The paper sets out the risk posed by AMR, highlights particular issues it raises for military operations.
>WHO World Health Organization. Antimicrobial resistance: global report on surveillance
http://www.who.int/drugresistance/documents/surveillancereport/en/. (2014). World Health Organisation.
Overview: Antimicrobial resistance (AMR) threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi. An increasing number of governments around the world are devoting efforts to a problem so serious that it threatens the achievements of modern medicine. A post-antibiotic era – in which common infections and minor injuries can kill – far from being an apocalyptic fantasy, is instead a very real possibility for the 21st Century.
This WHO report, produced in collaboration with Member States and other partners, provides for the first time, as accurate a picture as is presently possible of the magnitude of AMR and the current state of surveillance globally.
The report makes a clear case that resistance to common bacteria has reached alarming levels in many parts of the world and that in some settings, few, if any, of the available treatments options remain effective for common infections. Another important finding of the report is that surveillance of antibacterial resistance is neither coordinated nor harmonized and there are many gaps in information on bacteria of major public health importance.
Strengthening global AMR surveillance is critical as it is the basis for informing global strategies, monitoring the effectiveness of public health interventions and detecting new trends and threats. As WHO, along with partners across many sectors moves ahead in developing a global action plan to mitigate AMR, this report will serve as a baseline to measure future progress.
>Antimicrobial resistance, infection control and planning for pandemics: The importance of knowledge transfer in healthcare resilience and emergency planning
Jennifer Cole, Research Fellow, Emergency Management, Royal United Services Institute for Defence and Security Studies. Journal of Business Continuity & Emergency Planning
https://www.henrystewartpublications.com/
https://www.henrystewartpublications.com/jbcep/v6 Volume 6 Number 2 2012-13
>Antimicrobial stewardship: English Surveillance Programme for ...
11 Sep 2013 https://academic.oup.com/jac/article/68/11/2421/835268 by D Ashiru-Oredope
Programme for Antimicrobial Utilization and Resistance (ESPAUR) .... by antimicrobial resistance, as highlighted in the Report of the Chief
>The Commission's 2011 Action Plan against the rising threats from AMR
https://ec.europa.eu/health/amr/sites/amr/files/communication_amr_2011_7...
The Plan contains 12 actions for implementation with EU Member States and identifies 7 areas where measures are most needed:
- making sure antimicrobials are used appropriately in both humans and animals
- preventing microbial infections and their spread
- developing new effective antimicrobials or alternatives for treatment
- cooperating with international partners to contain the risks of AMR
- improving monitoring and surveillance in human and animal medicine
- promoting research and innovation
- improving communication, education and training